Processing of Requests for a change of health insurance
In the Slovak Republic, approximately 4 to 5% of insured people annually apply for a change in the health insurance company, which represents 200,000 – 250,000 requests. Insured persons can apply for a change of insurance company no later than 30th September if they want to be reinsured by 1st January of the following year. The process of acceptance of such requests is complex and insurance companies have long been dealing with it manually, which has resulted in a high level of error. The fact that 40% of applications came just before the end of the campaign also contributed to the high error rate. In addition to the error rate, the manual processing of requests also led to high costs of personal resources. Unconceptual communication with customers, as requests, often did not contain the correct data and attachments also led to a rising level of errors.
A comprehensive automation solution was designed in cooperation with the customer, who had an idea of how the process should look like. After analysing the issue, we came to a common solution that covered all campaign scenarios. Customer also collaborated with another company to carry out OCR of documents that clients sent to the customer. The processed documents by the OCR method are saved on a file server, where our application use the Folder Watcher tool to monitor a selected folder and, if it detects a new file, it initiates a new case of the requests processing.
The requests processing is automatic in the ideal scenario. Manual intervention is only required if an exception or error occurs. When an error occurs in it, the person who is responsible for the given part of the request processing is notified in the GUI (at the task). If the person decides that the error can only be corrected by the client’s input, he/she can notify the client directly from the system. Notification is done by e-mail. The client is notified if the request is incorrect, but also when the request is accepted. The client, if necessary, can add attachments to the request directly through the application. It will create a new case of the process of supplementing the attachments and then pair them with the existing request.
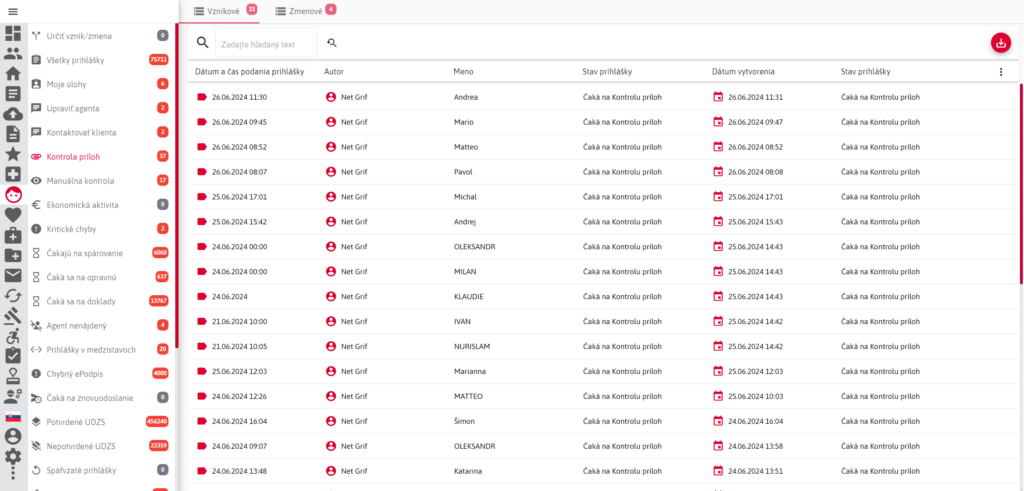
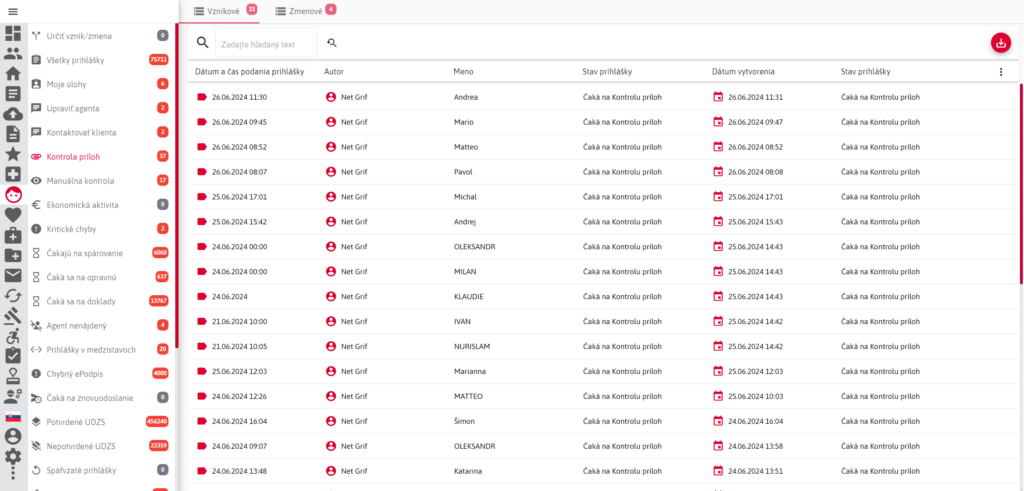
The link to the attachment completion process is sent directly to the client by e-mail notification. After the end of the processing, all files are stored on the DMS server of the insurance company, where the entire request is archived. Data is sent into the “Core” system. The client is listed as an insured person after confirmation by the “Core” system and the Health Care Surveillance Authority. Even after unsuccessful processing of a request, there is a record of the applicant in the system.
Integrations to individual systems are performed using SOAP or REST web services. REST web services are used to communicate with “Robots” or RPA modules serving the customer’s “Core” system. Besides, they were also used in the application for communication between the individual modules of our application, as some parts are public, but others are private. The SOAP web service is used for DMS server calls but also communication with the web services of the Health Care Surveillance Authority of Slovakia.
Up and running in 3 months
60 000 cases of requests within first month of production
200 000 cases of requests within first year of production
Significant reduction of error rate and manpower
The application was first put into production in August 2019. To date, it has been through many modifications. In addition to the processing of change requests, the system, after minor modifications, also began to be used for the processing of new insurance applications. The classic processing of paper requests has been extended to the processing of “Online” requests. This type of application also needed its own “Request Tracking” to make tracking of each request for employees easier. The application is currently deployed for more than a year and has started to implement the third campaign shift of processing requests.